Implantation of an artificial shoulder joint (shoulder prosthetics)
Causes
In most cases, the reason for the installation of a shoulder prosthesis is painful joint wear ("omarthrosis"), which is usually associated with a significant restriction of shoulder function.
Several factors can be responsible for the pronounced cartilage or bone wear between the humeral head and glenoid cavity.
In most cases, the wear and tear or destruction of the shoulder joint results from age-related and/or increased mechanical stress.
In addition, consequences of accidents (e.g. a fracture of the humeral head), older tendon tears (rotator cuff defects), circulatory disorders of the humeral head, chronic rheumatoid arthritis or premature wear due to chronic joint instability can be responsible for the development of omarthrosis.
left: X-ray image of an omarthrosis
right: X-ray of a healthy shoulder joint
Diagnostics
Clinical examination often reveals a painful restriction of shoulder movement. A reduction in strength of the shoulder or arm is also frequently detectable. Friction phenomena, so-called "crepitations", are conspicuous on examination.
X-rays can be used to reliably diagnose the extent of joint wear. In the case of severe osteoarthritis, for example, the joint space and the formation of jagged edges (osteophytes) can be detected. If additional damage to the tendons of the shoulder (rotator cuff) is suspected, ultrasound examination (sonography) or magnetic resonance imaging (MRI) can help clarify the situation.
Treatment
The main goal of treatment is to reduce pain and improve function, so that an improvement in the quality of life is achieved. The extent to which an improvement in the mobility of the joint is possible depends very much on the individual initial findings.
Depending on the individual situation, different types of prostheses are used:

 Surface replacement ("cap prosthesis" of the humeral head) in cases of mild omarthrosis and still well-preserved glenoid cavity
Surface replacement ("cap prosthesis" of the humeral head) in cases of mild omarthrosis and still well-preserved glenoid cavity
links: X-ray image of a cap prosthesis ("surface replacement")
right: cap prosthesis ("surface replacement", type "Durom" Fa. Zimmer)gkl
 Conventional stem prostheses for omarthrosis and acetabular wear
Conventional stem prostheses for omarthrosis and acetabular wear
right: anatomical shoulder prosthesis with glenoid replacement (Affinis type, Mathys company)
Short stem prostheses as modern implants for omarthrosis and acetabular wear
left: X-ray image of a short-shaft prosthesis
right: Short-shaft prosthesis (Affinis Short type, Mathys company)

 Special prostheses such as an inverse shoulder prosthesis (syn.: "Delta prosthesis", "Grammont prosthesis") for the combination of severe omarthrosis with joint instability and rotator cuff defects
Special prostheses such as an inverse shoulder prosthesis (syn.: "Delta prosthesis", "Grammont prosthesis") for the combination of severe omarthrosis with joint instability and rotator cuff defects
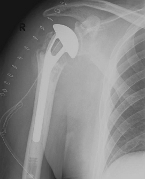
Right: radiograph of an inverse shoulder prosthesis for rotator cuff defect arthropathy.
left: Inverted shoulder prosthesis (Aequalis reversed type, Tornier company).

Fracture prostheses for complicated humeral head fractures
left: X-ray of a humeral head fracture before treatment with a fracture prosthesis.right: X-ray of a humeral head fracture after treatment with a fracture prosthesis
The inpatient stay is approximately 7 days, including the day of arrival before surgery.
After-care Treatment
Physiotherapeutic follow-up treatment begins on the first day after surgery and is individually adapted depending on the patient and the type of prosthesis used.
Patients receive an orthosis (bandage of the arm, "Gilchrist bandage") for 4 to 6 weeks. During this time, movement and weight-bearing on the arm are also deliberately restricted to ensure that detached tendons heal safely. This is followed by further physiotherapy aimed at restoring or improving strength and active mobility of the shoulder.










